EKG Tutorial—From Atoms to Arrhythmias
Overview.
This approach is different from what you may have seen before, shaped by a clinical path rooted in bedside nursing and critical care rather than traditional classroom instruction.
It emerged from years of caring for unstable patients, making real-time decisions, and needing the EKG to be a reliable clinical tool—not an abstract pattern to memorize.
It was built from the bedside, not from a template.
That bedside-first mindset was forged in the mid-1970s, when our Program Director stepped into one of the country’s earliest Cardiac Intensive Care Units and had to learn—quickly—how to make the EKG mean something for the patient in front of him.
n 1975, when our Program Director went to work in one of the first Cardiac Intensive Care Units in the country, he found himself electrocardiographically underwater. Within a year, he was one of those in charge of the unit.
This course distills what he learned—and more importantly, how he learned to think about the integration of the heart and its electrocardiogram.
It took thirty years to research and three years to write. You’ll master it far more quickly—and with vastly more depth—than those who rely on pattern memorization alone.
You will learn:
A three-step method to confidently analyze any cardiac rhythm.
A three-step framework for 12-lead ECG interpretation.
The why behind every waveform, traced all the way down to the cellular and atomic level.
This foundation is what makes the knowledge durable. It lasts. And it empowers clinicians—regardless of prior experience—to perform at a high level quickly and confidently.
Along the way, electrophysiology is continuously tied to cardiac hemodynamics and diagnostic decision-making, deepening how you think about cardiology as a whole.
On-Site Tutorial Info→
Perform Like the Most Successful Professionals in Your Field
Who Will Benefit.
This tutorial adapts seamlessly to a wide clinical audience, including:
Cardiac Care & Critical Care Nurses
Emergency & Critical Care Clinicians
ACLS Paramedics
Cardiovascular & Advanced Practice Sonographers
EKG Technicians
Medical Students, Interns, and Residents
Researchers seeking physiologic clarity behind ECG findings.
Whether you want rapid mental protocols, a deeper physiologic explanation, or both—this experience meets you where you are.
Learning Objectives.
Upon completion, participants will be able to:
Explain what’s actually happening inside the cardiac cell—and why those unseen events create the EKG changes you see at the bedside.
Understand how electrolytes, membrane dynamics, and fluid shifts affect cardiac electrical activity and rhythm stability.
Connect each EKG waveform to a specific phase of cardiac contraction, not just its appearance on paper or screen.
Trace electrical flow through the heart and anticipate how conduction problems will show up clinically.
Place electrodes correctly and interpret each lead’s viewpoint, improving signal quality and diagnostic confidence.
Quickly determine axis and recognize chamber enlargement, especially when findings change from baseline.
Recognize bundle branch blocks and fascicular blocks and understand when they matter clinically.
Use a reliable, step-by-step method to analyze any rhythm, even under time pressure.
Identify all degrees of AV block and anticipate their clinical implications.
Distinguish ventricular tachycardia from SVT with aberrancy when the difference affects immediate management.
Recognize pre-excitation patterns and pacemaker behavior, normal and abnormal.
Identify medication, electrolyte, metabolic, and physiologic effects that commonly alter EKG appearance—and know when to escalate concern.
Topics Include.
Atomic and molecular structure as the foundation of all EKG activity.
Diffusion, osmosis, and active transport—and what the EKG actually records.
The cardiac cell membrane and its role in electrical and mechanical activity.
How—and why—the conduction system directs electrical flow.
Systematic diagnosis of arrhythmias with speed and certainty.
A confident, repeatable method for 12-lead EKG analysis.
Recognition, differentiation, and localization of ischemia and injury.
Conduction delays, blocks, and pre-excitation mechanisms.
Pacemaker function and EKG evaluation.
Electrolyte imbalance and pharmacologic EKG effects.
Athletic conditioning and hypothermia patterns.
Guided, in-class analysis of rhythm strips and 12-lead studies.
Clinical Impact by Care Setting.
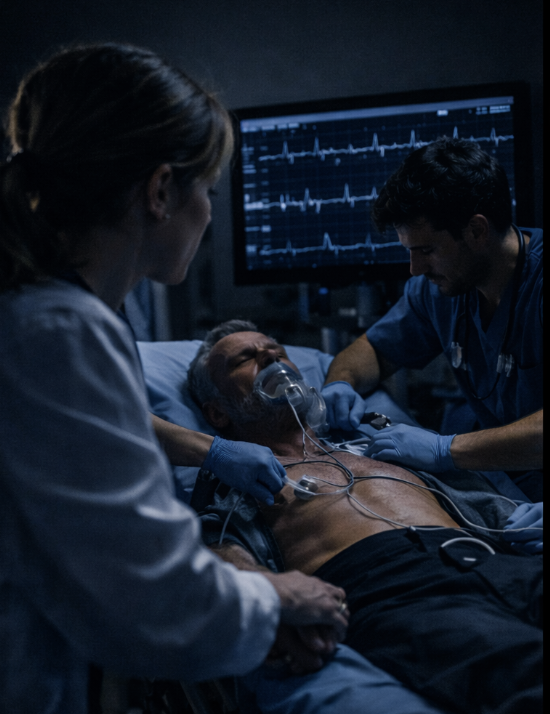
Why This Matters in the ICU/Critical Care.
When vasopressors and inotropes (norepinephrine, epinephrine, dopamine) alter heart rate, conduction, and myocardial oxygen demand.
When electrolyte shifts from renal failure, CRRT, or massive transfusion change repolarization before labs result.
When QT-prolonging medications (amiodarone, certain antibiotics, antiemetics) require rhythm awareness beyond a number on the monitor.
When temporary or permanent pacing modes (VVI, DDD, A-paced vs V-paced) must be distinguished from intrinsic rhythm changes.
When small EKG changes signal evolving ischemia or worsening physiology, not just monitor variation..
Why This Matters in the Emergency Room.
When the EKG is obtained before labs, imaging, or full history.
When pressors, push-dose meds, or sedatives affect rate and conduction in real time.
When QT-prolonging drugs intersect with electrolyte abnormalities in unstable patients.
When differentiating ventricular rhythms from paced or aberrant supraventricular rhythms changes immediate management.
When recognizing ischemia, injury, or conduction block accelerates triage and treatment ED nurses use the EKG as an early decision tool—not a retrospective report.
Why This Matters on Telemetry.
When patients are receiving beta-blockers, calcium channel blockers, or antiarrhythmics that subtly alter intervals and rate response.
When QT-affecting medications are added during the day shift and changes surface hours later.
When intermittent pacing spikes or capture changes appear and need to be recognized as device-related—not artifact.
When baseline abnormalities (BBB, AF, paced rhythms) make new changes easy to miss.
When accurate interpretation helps determine whether to escalate, re-evaluate leads, or continue observation.
Device Management | Pacemakers • ICDs • CRT
Recognize paced rhythms and distinguish atrial, ventricular, and dual-chamber pacing from intrinsic conduction
Identify loss of capture, loss of sensing, and fusion beats before they become hemodynamically significant
Differentiate paced tachycardia from ventricular tachycardia and other wide-complex rhythms
Recognize ICD-related EKG findings following anti-tachycardia pacing or defibrillation
Interpret CRT patterns and understand how resynchronization alters QRS width and cardiac efficiency
Know when an EKG change suggests device behavior versus evolving pathology
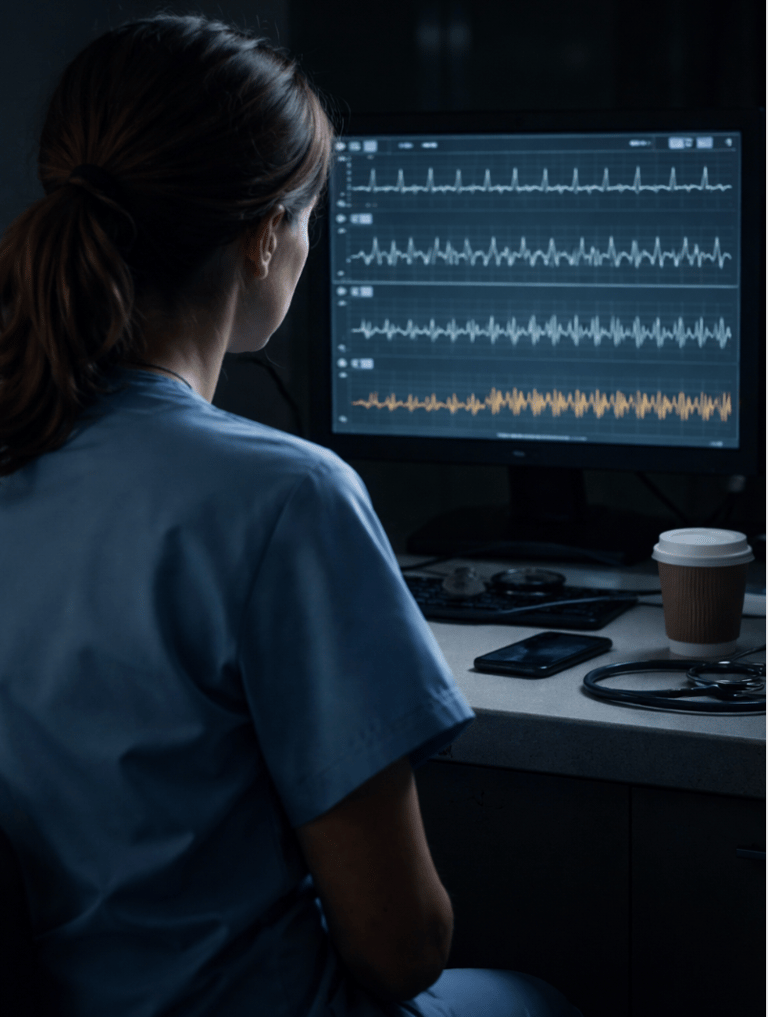
Why This Matters On Night Shift.
When it’s on you.
When consultants are off-site and answers aren’t immediate
When subtle rhythm changes happen quietly, before alarms sound
When medications, electrolytes, and fatigue intersect at 2:17 a.m.
When you’re deciding whether to watch, re-check, or wake someone up.
This course is built for those hours.
It teaches you how to understand what the EKG is telling you, not just recognize a shape on the screen—so you can trust your judgment, communicate clearly, and act with confidence when you’re the first, and sometimes only, line of recognition.
Because on nights, clarity matters more than speed—and understanding matters more than memorization.
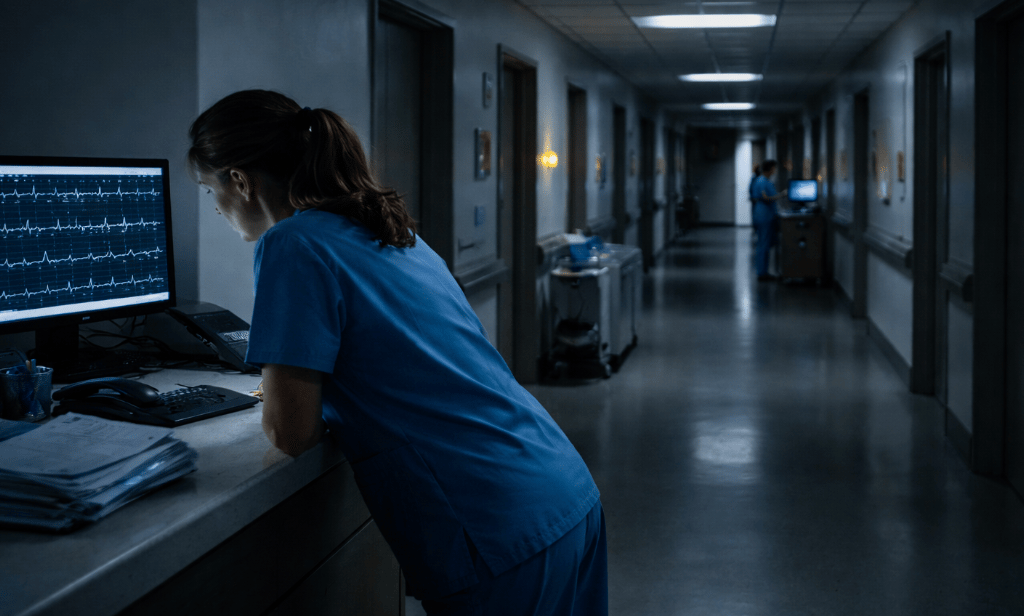

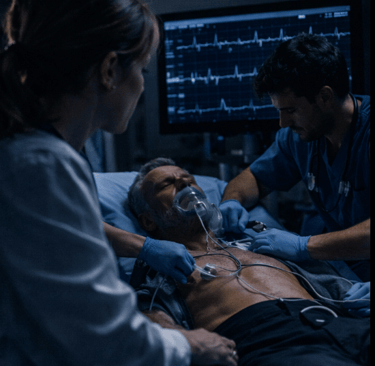





ICU nurses translate electrical signals into physiologic foresight.
ED nurses use the EKG as an early decision tool—not a retrospective report.
Telemetry nurses guard continuity and catch what others don’t see yet.
This course helps you interpret what the device is doing—so you can focus on what the patient needs.
On-Site Tutorial Info→
Training Clinicians Worldwide Since 1981.
Testimonials reflect individual learning experiences. Growth in skill and confidence develops through guided training, continued practice, and personal commitment.
Contact Us
(972 | 353-3200 USA Central Time
Course Campus:
4300 Wingren Drive
Irving (Las Colinas), Texas 75039
Mail | FedEx Address:
Box 101
Colleyville, TX 76034
Legal & Administrative
Privacy Policy
Accessibility Statement
© Keith Mauney & Associates Ultrasound Training Institutes MMXXVI. All rights reserved.
Courses & Learning
Your Skills-Building Experience
Hands-On POCUS- Point of Care Ultrasound
Hands-On Adult Echocardiography
Hands-On Transvaginal Pelvic Ultrasound
Ultrasound Physics
Cardiovascular Hemodynamics
EKG- From Atoms to Arrhythmias
